The opioid epidemic is one of the greatest public health challenges this century, and its deadly effects have only gotten stronger in recent years—the annual death toll rose from 8,000 deaths in 1999 to 50,000 in 2017. Multiple factors have contributed, including an increase in prescribing—often leading to overprescribing—and increased potency of opioids.
The current treatment landscape for opioid addiction mirrors that of other chronic diseases—it’s achieved with a balance of medication, counseling, and lifestyle changes—but how do we measure the impact of these interventions?
According to Jacob “Gus” Crothers, M.D., an addiction medicine specialist and the National Medical Director of Groups Recover Together (Groups), which operates about 70 addiction treatment sites across 11 states, real-world data (RWD) can be a powerful tool in assessing treatments for opioid use disorder (OUD).
Dr. Crothers’s past experience with addiction medicine spans industry, patient care, research, technology, and leadership roles, giving him a unique perspective on how different communities tackle OUD. Here, he shares perspectives on what the health care industry needs to know about addiction, the science behind OUD, and the research questions that real-world evidence (RWE) can address to help improve the delivery and outcomes associated with addiction care.
Responses have been edited for clarity and length.
Q: What should the health care industry, and the public more broadly, know about addiction?
A: First off, addiction is a chronic disease—a fact supported by data from the National Institutes of Drug and Alcohol Use. In a study comparing how addiction behaves compared to other chronic diseases, we see that the relapse rates for diabetes, hypertension, and asthma are similar to those of addiction. This is partly because it’s difficult to manage chronic conditions of any kind, but the stigma around relapse for other conditions is different than that for addiction relapse.
That said, addiction is a unique chronic disease. While the diagnostic criteria for most chronic diseases are purely biological, diagnostic criteria for most substance abuse disorders rely on one’s biological, psychological, spiritual, and social wellbeing.
Q: How do you measure the impact of the opioid epidemic on populations?
A: One way to measure its impact is in years of life lost. This is calculated by subtracting the age someone was when they died from the average life expectancy. Opioid use disorder is particularly terrible in this dimension, because it tends to kill people in their 20s, 30s, and 40s.
In 2016, there were about 1.6 million years of life lost to opioid use disorder in America. And it’s only gotten worse since then.
Part of the reason why OUD is becoming more and more deadly is because the epidemic is changing from less potent, prescription opioids to the more potent heroin, and now increasingly to ultra-potent fentanyl. This has led to many more unintentional overdoses and deaths.
Q: How do you account for population exposure to opioids?
A: The opioid epidemic is similar to a toxic exposure epidemic. Real-world data studies that describe the overall population exposure to opioids show that increased exposure leads to increased chance of addiction.
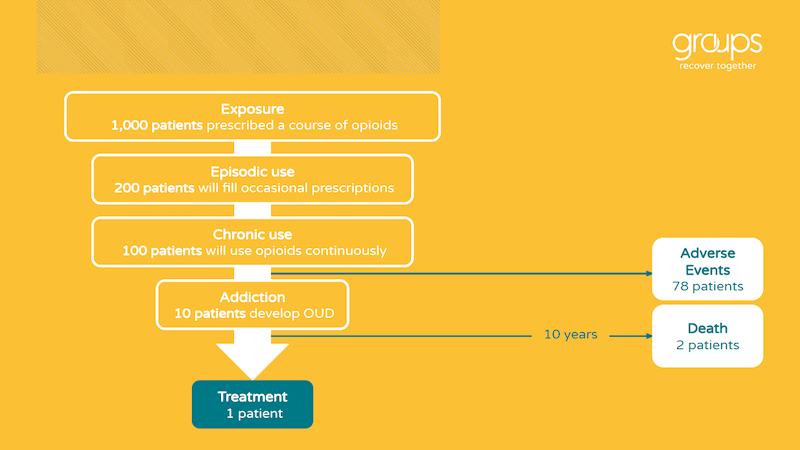
For every 1,000 patients who are prescribed a course of opioids, one in five will continue to fill occasional prescriptions. About half of them will become chronic users, meaning that their claims data shows one year later that they’re still filling opioids. And even if they take the medications as prescribed, about eight in ten patients prescribed opioids will experience an adverse event during their course of treatment.
About one in ten of people who are exposed chronically will eventually meet the criteria for addiction. And then, sadly, only about one in ten people who develop addiction will receive treatment. On average, patients don’t seek treatment until about ten years of suffering with the disease; over that same period, about two in ten will die.
Q: What does the current treatment landscape for opioid use disorder look like?
A: When managing any chronic disease, treatment relies on a long-term combination of medication, counseling, and lifestyle changes.
The medication options for opioid use disorder are methadone, buprenorphine (or Suboxone), and naltrexone (or Vivitrol).
Methadone is a full agonist; it’s the strongest and most dangerous, and because of that it’s the most highly regulated and the least convenient for a patient to take. It can only be dispensed at highly regulated opioid treatment programs.
Buprenorphine is a partial opioid agonist, meaning it is not as strong as a full agonist like methadone and thus significantly safer. It also has a ceiling effect, so even if the dose increases, the effect eventually levels off. This helps minimize the risk of overdose or adverse effects, but doesn’t impact efficacy. Because of that improved safety profile, it can be prescribed in the outpatient settings.
Naltrexone is a pure antagonist, but real-world data shows that it’s not as effective as the other two options. It’s the most convenient of the three, as it’s not highly regulated and not considered a controlled substance.
The goal with methadone and buprenorphine use is to find a dose that helps the patient feel “normal” and stabilize their physical and psychological symptoms while they work through counseling and lifestyle changes. RWE shows that the risk of relapse is extremely high if patients stop taking these medications, so it’s important that patients continue treatment as long as it takes to make significant progress in these other areas. But the absolute answer to “what is the optimal length of treatment” is unknown, and it’s a critical research question we need to pursue. It is the number one question that patients and providers ask me.
There are lots of counseling modality options, but there’s no correlation in the data between the level of treatment intensity and the level of efficacy. For example, a 30-day residential treatment center stay with commercial insurance costs about $50,000 for the payer, but has a very low rate of efficacy.
Options for lifestyle changes are diverse, but it boils down to people, places, things, and behaviors. The lingo in the industry is: “the only thing you have to change is everything.”
Q: What do outcomes for OUD treatment look like?
A: The outcomes for opioid use disorder are sobering. OUD has a two percent mortality per year, which may sound low, but with an age-matched control that totals to 15 times the mortality of the general population. Long-term follow up studies show that after ten years, roughly 20 percent of people addicted to opioids are deceased, and less than 30 percent are long-term abstinent. There are high rates of incarceration, low rates of quality of life, and many complications like HIV and hepatitis C.
The data continually shows that treatment works, but the challenge is keeping people engaged in efficacious treatment. According to the patient-reported outcomes Groups has collected internally, we see that people in our program experience a tremendous improvement in their quality of life while in treatment, and achieve clinical outcomes at two to four times the industry standard. We see that 65 percent of Medicaid patients and 76 percent of commercially insured remain engaged in treatments after six months, compared to the industry standards of 25 percent and 30 percent respectively. We also see an 89 percent attendance compared to 20 percent industry average, and 90 percent abstinence versus 18 percent.
Q: What trends do you see in the data regarding today’s treatment landscape?
A: The treatment landscape is moving from a crisis of access to a crisis of quality. Although access is improving, there are still many unanswered questions around treatment supply. Much of this has to do with policy; a primary care physician has to jump through extra hoops to treat addiction, but not to treat pain.
We can look to other countries that see better outcomes for different approaches: Canada allows patients to receive methadone at the pharmacy (rather than a highly-regulated opioid treatment program), France makes buprenorphine easier to access, and Portugal has decriminalized most drug use and funneled that energy into treatment. The U.S. has lots to learn around how to pay for the treatments that work.
A big question right now is around telemedicine. It has a tremendous opportunity to expand access, but there’s still a need to increase access to and quality of treatment. Our internal data is showing that telemedicine works—we’re seeing consistent results between our telemedicine cohort and a historical in-person cohort’s weekly session attendance, abstinence, and retention rates.
Q: How can RWD help improve the understanding of OUD to support better patient outcomes?
A: Real-world data can help answer questions around treatment effectiveness. We have access to claims data on medication doses and formulations, but we don’t know what combinations, lengths of time, or dose intensity and frequency work best to help someone achieve stability such that they can eventually taper off their medication. That is the number-one question every patient and every doctor wishes we could answer.
There are also challenges with measuring the impact of psychosocial treatments; an hour of counseling at one clinic is not necessarily the same as an hour of counseling at another clinic. Patient-reported outcomes can be a key resource to contextualize these data.
Smartphone data could be the wave of the future to measure lifestyle changes. We have the ability to responsibly gather information about a person’s disease course, and to—again, responsibly—use this information to inform what combination of treatments helps people stay sober.
In terms of new frontiers, buprenorphine was a breakthrough for the industry. Can we find another molecule that’s even safer? There’s also much to explore in terms of opioid receptors—opioid receptors are present on almost every tissue in the body, but we have a limited understanding of what they do. There’s also an opportunity to develop immunizations against addictive substances: a cocaine vaccine, a fentanyl vaccine, etc. That will open up all sorts of interesting ethical and clinical questions that RWD can help address.

